Mental Health & Diet
Improve The Gut & The Brain With Plant Based Nutrition
Each day mental health awareness is on the page of every newsfeed on the internet and in the newspapers. Bill and I have worked with clients and students for decades who have suffered from many mental health problems. The suffering could have been the result of them losing a loved one, a diagnosis of some terminal illness, the loss of their home, job or any other multitude of things that humans are challenged with daily. I am not suggesting you can wave a magic wand and heal your pain by changing your diet but connecting the gut/brain to mental health is a new and fascinating area of research.
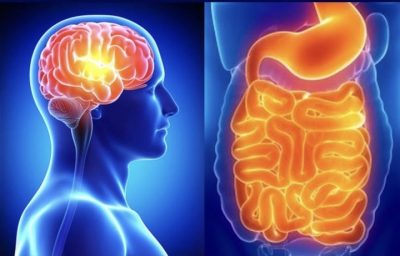
The Gut-Brain Connection
The gut-brain connection is recognised as a basic tenet of physiology and medicine. There is no shortage of evidence of gastrointestinal involvement in a variety of neurological diseases. What has been discovered is that gut bacteria can play a significant role in your psychology and behaviour as well as your digestion. This is why nourishing your gut flora is extremely important. What a surprise, we have two brains, one inside your skull and one in your gut, and each needs its own vital nourishment.
These two organs are actually created out of the same type of tissue. This is why your intestinal health can have such a profound influence on your mental health, and vice versa. As a single system, the gut and brain are working together to keep your body functions operating at peak condition. They use the same methods and nerves to communicate. In fact, your “second brain” has all the same neurotransmitters and just as many neurons as the spinal cord or peripheral nerves. Almost 95% of your body’s serotonin are located in your gut. This is the neurotransmitter that helps regulate mood and social behaviour, appetite and digestion, sleep, memory, and sexual desire and function.
Clinical Depression
According to the World Health Organization, more than 264 million people of all ages suffer from depression[1]. It is one of the leading causes of disability worldwide and a major contributor to the global burden of disease making it a leading cause of losing healthy years of life as a result of disability. Why is depression so common? Aside from the foregoing, diet plays a huge role in mental health once we learn that our gut is in fact our second brain.
My friend, Dr. Michael Greger explains that the relationship between mental health and inflammation was first noted in 1887. The doctor who discovered this relationship was Julius Wager-Jauregg, the only psychiatrist to have ever won the Nobel Prize. Since that time more studies have shown the importance of this fact.
The modern diet is massively pro-inflammatory. Every client who comes to us for health counselling has a hotbed of inflammation in their colon. Literally, if your gut is “on fire,” your entire body is under attack and heading for many diseases. This inflammation directly irritates the Vagus nerve, the direct connection between the gut and the brain. The mechanism of result has been detailed in many studies[1] [2] and the results are the same. Our gut biome (the colonies of microorganisms that live in the gut) can be contaminated by the food we eat. The prime culprits are found in the modern diet.
Inflammation and Diet
The foods that most exacerbate inflammation are those that are mostly present in modern processed foods. They include simple sugars, fructose, dairy foods, eggs, alcohol, meat, hydrogenated fats, palm oil and some fruits and vegetables such as tomato and pineapple. These foods are not only causal in disrupting the gut biome but if there is any inflammation in the body, they can feed the process.
Using data from two large studies[3], Danish researchers have found that higher blood levels of C-reactive protein, or CRP, are associated with a greater risk of psychological stress and clinical depression. Eating a diet with significant amounts of animal protein causes a burst of inflammation that can increase symptoms in an already depressed person. By eating a diet rich in antioxidants, a plant-based diet, has a profound benefit in stress reduction.
This is good news since the gut biome changes with your diet. A plant-based diet can cut the C- reactive protein by 30% within two weeks because of the anti-inflammatory properties of antioxidants. This is important since clinical depression can be accompanied by increased oxidative stress and the autoimmune inflammatory responses it creates.
Going vegan has multiple proven benefits. An exclusively plant-based diet is naturally higher in fibre and boosts bacteria that make short-chain fatty acids. These SCFAs improve immunity against pathogens, provide an energy source for our gut lining, maintain the blood-brain barrier, activate critical intestinal protection mechanisms, and help control our blood sugar and caloric intake.
Fermented Foods Are The Best Route To Optimal Digestive Health
Fermented foods have been traditional staples in most cultures, but modern food manufacturing has eliminated most of these foods. You can find traditionally fermented foods like miso soup, tempeh, naturally fermented soy sauce, sauerkraut or kimchi to feed your gut biome. When clients taste my ‘miso broth’ and fermented vegetables their eyes light up. Miso soup should be a daily staple. Happy gut - happy me.
Self-Help Tips To Do At Home
For congestion in the lungs try steamed greens and ginger – the steamed greens move energy up and the ginger moves energy out. Steam the greens until vibrant green and then squeeze some freshly grated ginger juice on top. Also, try parsley tea – the parsley moves energy up and out. Add a few sprigs of parsley to a cup of boiling water. Leave to infuse 5 minutes. Drink and eat the parsley.
Doing exercises that open up the chest and shoulder areas can get the lung energy moving again, as well as breathing exercises. It seems so silly to say it, but if you want to get healthy lungs there is one thing you must do – breathe! Doing aerobic exercises, such as fast walking, bicycling and swimming, is great. Here is an easy and effective way to energise not only the lungs, but the whole of the body.
Join Bill and I in service for a healthy world for humans and nonhumans alike. How to eat right and save the planet drives us both daily.
In good health
[1] Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol. 2016 Jan;16(1):22-34. doi: 10.1038/nri.2015.5. PMID: 26711676; PMCID: PMC5542678.
[2] The role of inflammation and the gut microbiome in depression and anxiety. Jason Peirce, Karina Alvina, 29 May 2019 – Journal of Neuroscience Research
[3] Brain, Behaviour and Immunity. 2017 May;62:344-350. doi: 10.1016/j.bbi.2017.02.020. Epub 2017 Mar 1.
Association between C-reactive protein (CRP) with depression symptom severity and specific depressive symptoms in major depression.
[1] WHO fact sheet on depression, January 2020


